As the COVID-19 pandemic drags on into 2022, we should not keep doing the same thing over and over again, expecting a different result. If a general is losing the war, he is replaced.
Current control measures have not worked, despite their enormous cost and the destruction of livelihoods, education, usual medical care, and hope. The promised vaccines have not brought relief. All-cause mortality is increasing as more people get vaccinated, not decreasing as would be expected with a safe and effective vaccine.
HOSPITAL CRISIS
Hospitals are being overwhelmed, largely because of inadequate staffing. Despite this, dedicated and experienced staff are being terminated because they decline the COVID injections—even if they have demonstrated natural immunity. If staff morale is low, could it be because workers feel that dedication is not valued, their own professional judgment is disrespected, and their own health is less important than vaccination statistics?
Burnout is epidemic. A key cause is moral injury, which occurs when people are forced to act in ways they believe to be immoral. Hospitals are enforcing rigid protocols, even when ineffective or harmful, despite patients’ objections and pleas to try something different. Any who deviate will most likely be terminated and possibly kept from working in medicine ever again.
Formerly popular “shared decision-making” is thrown out with respect to COVID-19. Hospitals may insist on giving remdesivir despite poor evidence of effectiveness and a high incidence of renal failure and other serious adverse effects. Hospitals may absolutely refuse to try anything not in their restricted protocols even though patients are dying. Doctors may assert that “there’s no [CDC-accepted] evidence that that works,” while there is clear evidence that what they are doing does NOT work in a particular real patient.
There is substantial evidence, summarized at c19study.com, that many treatments (vitamin C, vitamin D, ivermectin, hydroxychloroquine, and several others), especially if started early in sequenced combinations, reduce morbidity and mortality. Results are far better than with remdesivir, and without complications such as multiple organ failure. The electronic health record is supposed to allow us to tell “what works.” And if staff members were permitted to speak freely without fear of retaliation, they could share observations and scientific publications. Hospitals, however, are blocking queries or communications not supportive of their predetermined opinions.
INFECTION CONTROL MEASURES
Masking and distancing mandates have not worked. Regions with more rigorous restrictions are not doing better. What about requiring N95 masks? N95 masks are more effective than surgical masks IF they are properly fitted. This is a process that takes at least 15 minutes. Men need to be clean-shaven—even a one-day stubble can interfere with fit. These masks impair gas exchange and can cause acid-base imbalances. Thus, they cannot be tolerated for prolonged periods.
N95 masks produced by 3M 10 years ago were all stamped In bold large print: “WARNING: This respirator helps protect against certain particles. Misuse may result in sickness or death.” Currently manufactured masks do not carry this warning, but there is no evidence that they are safer.
Airborne respiratory viruses can also enter through the conjunctiva, so eye protection is as important as masks in high-risk exposures.
Mandatory vaccination or constant pressure to get vaccinated and boosted according to the prevailing recommendations, say with every visit to a medical facility, is advocatedby authorities from the Biden Administration down to local levels. People freely choose to be vaccinated to reduce the risk of severe illness or death from COVID-19. However, mandatory vaccination is not justified on public-health grounds:
- The COVID-19 vaccines are not demonstrated to prevent infection or transmission.
- The current vaccines may offer no protection against new variants.
- The Vaccine Adverse Event Reporting System (VAERS)—our early warning system, is signaling an unprecedented rate of death and permanent disability following vaccination. For persons at low risk of death from COVID, vaccination risk may well exceed potential benefit.
- The long-term effects of these novel genetically engineered vaccines cannot be known. These could include cancer, autoimmune disease, infertility, birth defects, immune deficiency, or antibody-enhanced disease.
WHAT COULD WE DO DIFFERENTLY?
Instead of the bipartisan but highly politicized failing agenda of test, mask, isolate, vaccinate, and boost, policymakers should consider the following:
Infection-control measures that would also be of benefit in other infectious conditions, but are generally neglected, include:
- Far-ultraviolet (far UVC) air purification, even in occupied areas; air filtration with HEPA filters and UV exposure; disinfecting clinic or hospital rooms and public transportation with ozone;
- Reducing viral load with povidone iodine or other mouthwashes, gargles, and nasal sprays.
Pre- and post-exposure prophylaxis, as is now routine for HIV, is appropriate for both vaccinated and unvaccinated individuals. This overlaps with early treatment. Some health workers report that very few seriously ill individuals in the hospital had had early out-patient treatment. Access to monoclonal antibodies has been difficult, and these may be of reduced effectiveness against new variants. The medical community is not informing people of the need for adequate levels of vitamin D and zinc. Prescriptions for hydroxychloroquine and ivermectin are discouraged, despite theoretical and clinical support for their use and an excellent long-term safety record. Regulatory agencies are impermissibly interfering with physicians’ prescribing, pharmacists’ dispensing, and access to over-the-counter agents such as N-acetyl cysteine (NAC).
Preserving our hospitals requires recognizing and mitigating the reasons why they are overwhelmed. These include: vaccine mandates; an unprecedented influx of migrants who are not medically screened; refusal of early treatment to ambulatory patients until seriously ill enough for admission; and government policies that force shutdown of remunerative services just in case more COVID beds are needed, so that reserve capacity is lost.
I would appreciate the opportunity to discuss these issues with you further.
Respectfully yours,
Jane M. Orient, M.D. Executive Director, Association of American Physicians and Surgeons


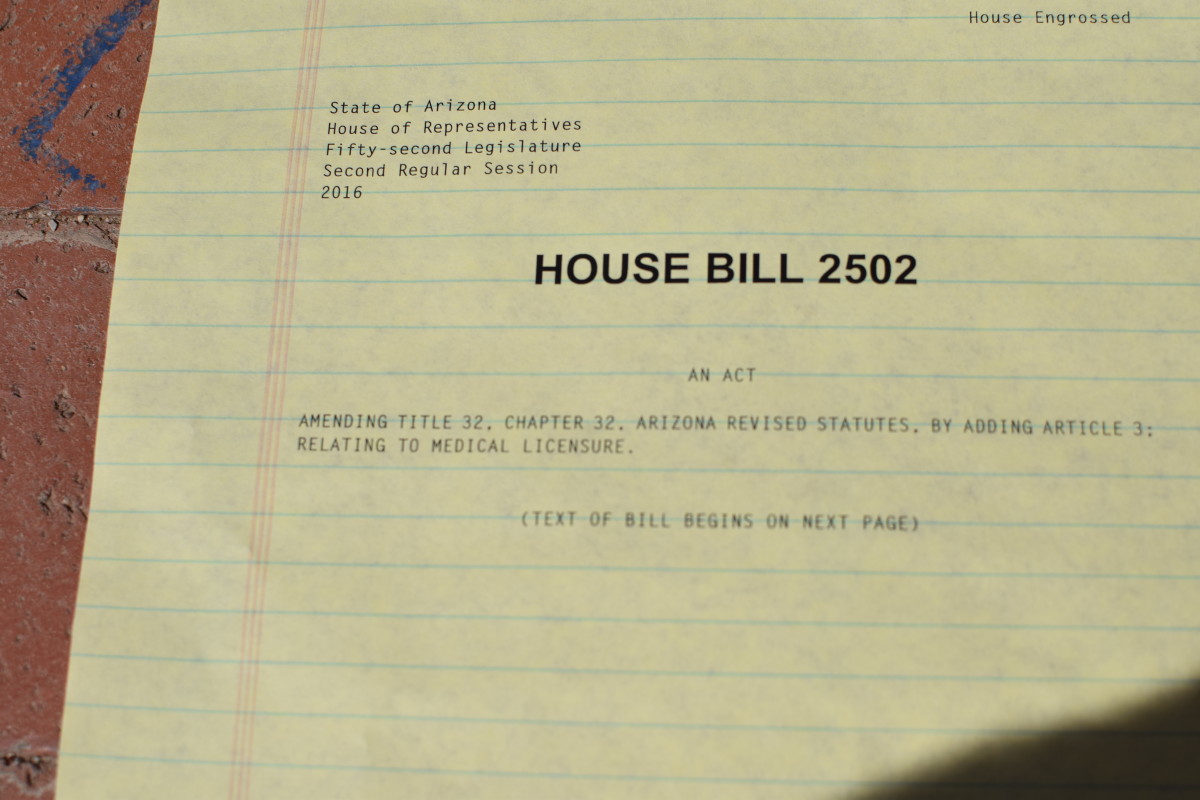

 Is a “free trade zone” for medical care possible in the U.S.? Join us on March 9, 2016 for dinner and a presentation by Twila Brase, founder of the Citizens’ Council for Health Freedom (CCHF). She will review CCHF’s Wedge of Health Freedom, an innovative free-market health care solution that will defuse Obamacare.
Is a “free trade zone” for medical care possible in the U.S.? Join us on March 9, 2016 for dinner and a presentation by Twila Brase, founder of the Citizens’ Council for Health Freedom (CCHF). She will review CCHF’s Wedge of Health Freedom, an innovative free-market health care solution that will defuse Obamacare.